OVERVIEW
Despite pain and sleep disturbances being primary reasons for medicinal cannabis use, the effects of cannabis and chronic pain on sleep architecture have been studied mainly in isolation.New BrainHealth research aims to create an integrated understanding to guide treatments and minimize risks in this population. Led by Tracy Brown, a UT Dallas cognition and neuroscience PhD student working in Dr. Francesca Filbey's Laboratory of Neuroimaging of Reward Dynamics, the study seeks to determine the interactive effects of regular cannabis use on chronic pain and sleep.A total of 339 nights (2273.43 hours) of in-home sleep electroencephalogram (EEG) recordings were collected from 60 adults (32% self-reporting chronic pain and 47% self-reporting cannabis use) over seven consecutive nights per participant. A mixed-model repeated-measures ANCOVA tested the main effects and interactions of chronic pain and regular cannabis use on total sleep time (TST), total slow-wave sleep (SWS), total rapid-eye-movement (REM), sleep onset latency (SOL), and number of awakenings.Results indicate a significant main effect of cannabis use on SWS, TST, SOL and REM. Significant interactions emerged between cannabis use and chronic pain on SWS and REM sleep, indicating a tradeoff. Increased SWS comes at the cost of less REM sleep – the kind of sleep that is critical for emotional regulation and memory integration. Additionally, while cannabis may initially enhance SWS, benefits diminish with chronic use. These findings may reflect a dysregulated sleep response in individuals using cannabis to manage chronic pain, highlighting the need to consider both beneficial and detrimental effects of cannabis on specific sleep stages.The figures below demonstrate mean (± SE) change in SWS and REM duration. In those with no pain, SWS decreased 1.19% and REM decreased 1.88% with cannabis use. In those with chronic pain, SWS increased 6.00% and REM decreased 8.85% with cannabis use.
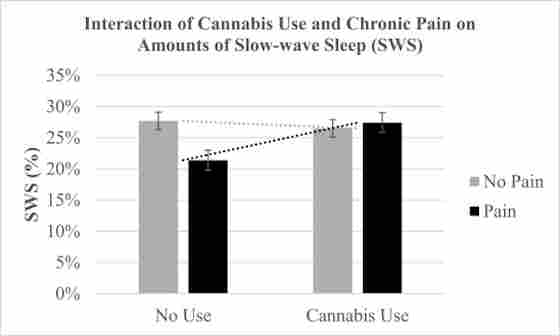
Figure 1. The interaction of regular cannabis use and chronic pain on the percentage of slow-wave sleep (SWS). The mean (SE) values were 27.41% (.02) for chronic pain and cannabis use, 26.49% (.01) for no pain and cannabis use, 27.68% (.01) for no pain and no cannabis use, and 21.41% (.02) for chronic pain and no cannabis use.
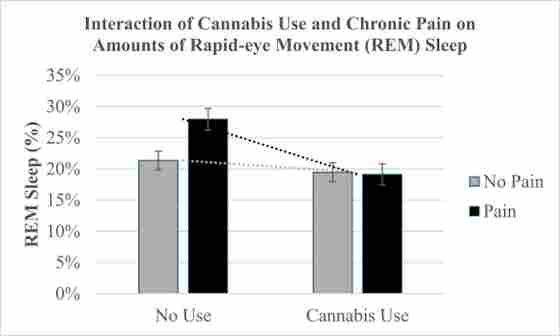
Figure 2. The interaction of regular cannabis use and chronic pain on the percentage of rapid-eye movement (REM) sleep. The mean (SE) values were 19.11% (.02) for chronic pain and cannabis use, 19.47% (.02) for no pain and cannabis use, 21.35% (.02) for no pain and no cannabis use, and 27.96% (.02) for chronic pain and no cannabis use.




